Medical Eye Disease
External Eye Disease
An increasing number of eye allergy cases are related to medications and contact lens cleaning solutions. Also, animal hair and certain cosmetics, such as mascara, face creams, and eyebrow pencil, can cause allergies that affect the eye. Touching or rubbing eyes after handling nail polish, soaps, or chemicals may cause an allergic reaction. Some people have sensitivity to lip gloss and eye makeup. Allergy symptoms are temporary and can by eliminated by avoiding contact with the offending cosmetic or detergent.
- Blepharitis is a chronic inflammation of the eyelids and is one of the most common disorders of the eye. Oils and other secretions build up on the eyelid surface and eyelashes, resulting in red, flaking or crusting of the eyelids. Other symptoms can include a sandy, gritty sensation, with burning, itching and/or redness. Although blepharitis is a chronic problem, applying warm compresses and lid scrubs can help control it. In some cases, it may be necessary to prescribe an antibiotic ointment.
- Warm compresses – soak a clean washcloth in very warm water, squeeze out the excess water, and then press it against your closed eyelids for approximately five minutes. You may need to rewarm the cloth several times. This will help to soften and loosen the debris on the eyelids.
- Lid scrubs – following the warm compresses, gently clean the eyelid margin (at the base of your lashes) with the edge of the washcloth using a side-to-side motion. You may use solution with a small amount of baby shampoo to cleanse your eyelids, or use a pre-packaged eyelid scrub solution.
- The above treatment should be repeated two to four times daily for the first two or three weeks. As your symptoms improve, you can decrease the frequency as necessary to maintain your comfort level. Remember this is a chronic condition and stopping treatment altogether may result in a recurrence of symptoms. Both topical and oral medications may be required initially to help get this condition under control.
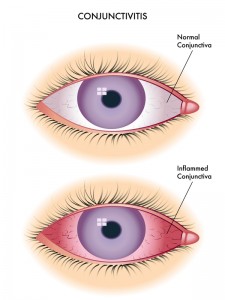
- Conjunctivitis is an inflammation of the conjunctiva, the thin, transparent layer that lines the inner eyelid and covers the white part of the eye.
- The three main types of conjunctivitis are infectious, allergic and chemical. The infectious type, commonly called “pink eye,” is caused by a contagious virus or bacteria. Your body’s allergies to pollen, cosmetics, animals or fabrics can also bring on allergic conjunctivitis. And, irritants like air pollution, noxious fumes, or chlorine in swimming pools may produce the chemical form.
- Common symptoms of conjunctivitis are red watery eyes, inflamed inner eyelids, blurred vision, a scratchy feeling in the eyes and, sometimes, a pus-like or watery discharge. Conjunctivitis can sometimes develop into something that can harm vision so you should see your Optometrist promptly for diagnosis and treatment.
- The best way to treat allergic or chemical conjunctivitis is to avoid the cause. If that is not possible, prescription or over-the-counter eye drops may relieve discomfort. Infectious conjunctivitis, caused by bacteria, can be treated with antibiotic eye drops. Other forms, caused by viruses, cannot be treated with antibiotics. They must be fought off by your body’s immune system.
- To control the spread of infectious conjunctivitis, you should keep your hands away from your eyes, thoroughly wash your hands before applying eye medications and do not share towels, washcloths, cosmetics or eye drops with others.
What is dry eye?
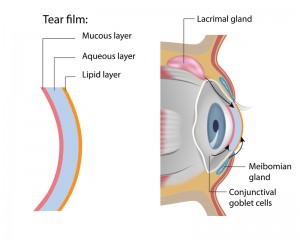
- The tear film consists of three layers – an outer, oily (lipid) layer that keeps tears from evaporating too quickly and helps tears remain on the eye; a middle (aqueous) layer that nourishes the cornea and conjunctiva; and the inner (mucin) layer that helps to spread the aqueous layer across the eye to ensure that the eye remains wet. As we age, the eyes often produce fewer tears. Also, in some cases, the lipid and mucin layers produced by the eye are of such poor quality that tears cannot remain in the eye long enough to keep the eye sufficiently lubricated.
- The continuous production and drainage of tears is important to the eye’s health. Tears keep the eye moist, help wounds heal, and protect against eye infection. In people who have dry eye, the eye produces fewer or less quality tears and is unable to keep its surface lubricated and comfortable.
What are the symptoms of dry eye disease?
- The most common symptoms of dry eye are usually a scratchy or sandy feeling, as if something is in the eye. Other symptoms may include stinging or burning of the eye; episodes of excess tearing that follow periods of very dry sensation; a stringy discharge from the eye; and pain and redness of the eye. Sometimes people with dry eye experience heaviness of the eyelids or blurred, changing, or decreased vision, although loss of vision is uncommon.
- Surprisingly, some people with dry eye may have tears that run down their cheeks. This is because the eye may be producing less of the lipid and mucin layers of the tear film, which help keep tears in the eye. When this happens, tears do not stay in the eye long enough to thoroughly moisten it.
What causes dry eye disease?
- Dry eye can occur in any climate, as can be made worse with the use of some drugs, including antihistamines, nasal decongestants, tranquilizers, and anti-depressants. Dry eye is more common in women, especially after menopause. People with dry eye should let their health care providers know all the medications they are taking, since some of them may intensify dry eye symptoms.
- People with autoimmune diseases, such as rheumatoid arthritis, can also develop dry eye. It is important to note that dry eye is sometimes a symptom of Sjögren’s syndrome, a disease that attacks the body’s lubricating glands, such as the tear and salivary glands. In this case, a complete physical examination may diagnose any underlying diseases.
How is dry eye disease treated?
- Artificial tears, which lubricate the eye, is generally the initial treatment for dry eye. They are available over-the-counter without a prescription. Sterile ointments are sometimes used at night to help prevent the eye from drying. Using humidifiers, wearing wrap-around glasses when outdoors, and avoiding windy and dry conditions may bring relief. For people with severe cases of dry eye, temporary or permanent closure of the tear drain (small openings at the inner corner of the eyelids where tears drain from the eye) may be helpful.
- Some people may find relief by supplementing their diets with omega-3 fatty acids, which are found naturally in foods like oily fish (salmon, sardines, anchovies) and flax seeds.
- If these methods fail, your Optometrist may suggest use of a prescription medication. One such medication, cyclosporine (Restasis®), works by stimulating tear production and reducing inflammation. Steroid eye drops may also be used, but are generally not recommended for long-term treatment.
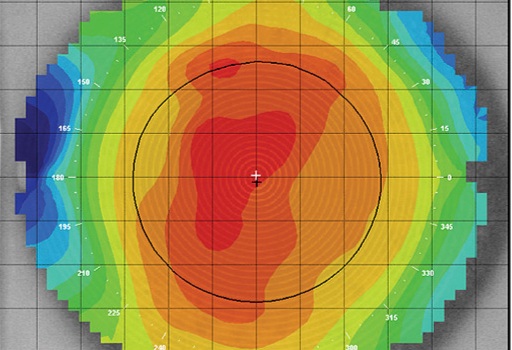
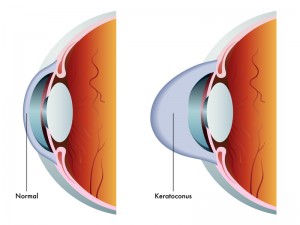 In keratoconus, the normally round cornea becomes progressively thinner and weaker, causing it to bulge outward in the middle and change to a cone shape. This can cause vision problems that range from moderate to severe astigmatism and nearsightedness, as well as swelling and scarring of corneal tissue. Although the cause of keratoconus is unknown, there may be a hereditary link, and appears to happen more frequently to individuals who vigorously rub their eyes. The disease usually presents in adolescence.
In keratoconus, the normally round cornea becomes progressively thinner and weaker, causing it to bulge outward in the middle and change to a cone shape. This can cause vision problems that range from moderate to severe astigmatism and nearsightedness, as well as swelling and scarring of corneal tissue. Although the cause of keratoconus is unknown, there may be a hereditary link, and appears to happen more frequently to individuals who vigorously rub their eyes. The disease usually presents in adolescence.
Depending on how far the disease has progressed, keratoconus treatment may include:
- Glasses: These may be used early in the progression of keratoconus to correct vision issues.
- Contact lenses: There is no one design that is best for every type or stage of keratoconus. The “best lens” is the one that fits your eye, corrects your vision and is comfortable to wear. At Mt Baker Vision Clinic, our doctors are highly experienced contact lens fitters for the irregular cornea, and will work tirelessly to select the best lens for your eye. A great deal of patience is required both on the part of the fitter and the patient.
- Scleral Lenses: Recently, because of improved contact lens material and design technology, scleral lenses have become a great option for many folks with irregular corneas, including keratoconus. These are large diameter lenses that rest on the white part of the eye, called the sclera, and vaults over the cornea. The size can be an alarming prospect for some, but scleral lenses have many advantages. Because of their size, they do not fall out, and dust or dirt particles cannot get under them during wear. They are surprisingly comfortable to wear because the edges of the lens rests above and below the eye lid margins so there is no lens awareness. Dr. Koning has a particular enjoyment and patience for fitting this type of lens.
- Corneal transplant: If the disease progresses to the point where none of the typical treatments work, corneal transplant surgery may be required. Two kinds of corneal transplants exist: full and partial.
- Corneal Collagen Cross-linking (sometimes abbreviated CCC, or CXL): There is currently a multicenter clinical trial of this novel treatment for keratoconus and other corneal ectasias. This clinical trial is investigating corneal collagen cross-linking, a treatment designed to delay the progression of keratoconus and corneal ectasia by strengthening corneal tissue.
Internal Eye Disease
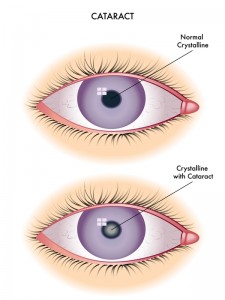
- Cataracts develop slowly and painlessly. Vision in the affected eye(s) slowly gets worse. Mild clouding of the lens often occurs after age 60, but it may not yet cause any vision problems. According to the National Institute of Health, most people have cataracts that affect their vision by age 75.
- Problems with seeing may include:
- Being sensitive to glare
- Cloudy, fuzzy, foggy, or filmy vision
- Difficulty seeing at night or in dim light
- Doubled vision in one eye
- Loss of color intensity
- Problems seeing shapes against a background or the difference between shades of colors
- Seeing halos around lights
- Frequent changes in eyeglass prescriptions
- Cataracts lead to decreased vision, even in daylight. Most people with cataracts have similar changes in both eyes, though one eye may be worse than the other. Often there are only mild vision changes.
- The only definitive treatment for a cataract is surgery to remove it. If a cataract is not making it hard for you to see, surgery is usually not necessary. Cataracts do not harm the eye, so you can have surgery when you and your Optometrist decide it is right for you. Surgery is usually recommended when you cannot do normal activities such as driving, reading, or looking at computer or video screens, even with glasses.
- The best prevention involves controlling diseases that increase the risk of a cataract. Avoiding exposure to things that promote cataract formation can also help. For example, if you smoke, now is the time to quit! Also, when outdoors, wear sunglasses to protect your eyes from UV rays.
- Vision typically improves dramatically after cataract surgery. If other eye diseases, such as macular degeneration, are present, vision may not improve to 20/20. Your eye doctor at Mt Baker Vision Clinic can help you determine this in advance.
- Glaucoma is a group of diseases that can steal sight without warning or symptoms. Statistics released and reported by the Glaucoma Research Foundation indicates that over four million Americans have Glaucoma… and only half are aware they have it!
- Glaucoma is one of the leading causes of blindness in the U.S. It most often occurs in people over age 40, but can also strike about 1 out of every 10,000 babies born in the U.S. Young adults can also get Glaucoma. African-American’s are particularly susceptible at a younger age.
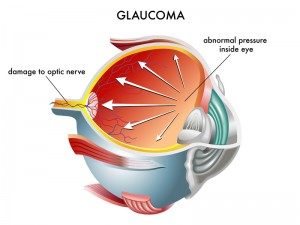
- Glaucoma damages the optic nerve at the back of the eye. Generally, the internal pressure of the eye to increase enough to damage those nerve fibers in the optic nerve and cause vision loss. The increase in pressure occurs when the outflow passages that normally allow the outflow of fluid in the eyes to drain become clogged or blocked.
- Open angle glaucoma, which is the most common type of glaucoma, develops gradually and painlessly, without symptoms. As the disease progresses, a person with glaucoma will not notice any symptoms until late in the disease when vision gradually fails with: blurred vision, loss of peripheral vision, difficulty focusing on objects, and sometimes the presence of halos around lights.
- Glaucoma is a misunderstood disease, and it is extremely important to note that glaucoma is painless and can cause blindness if it is left untreated. We do not say this to frighten or upset you, but because we want to be sure you understand. Glaucoma is not curable yet, but the goal is to stabilize the condition. Unfortunately, vision loss cannot be regained. The important first step to preserving your vision is diagnosis and control through eye exams. This will hopefully allow prevention of vision loss, which is why we encourage everyone to come in for a thorough annual eye exam.
- Know that Glaucoma cannot be prevented, but if diagnosed and treated early, it can be controlled. Many people wonder why we dilate their eyes. Receiving an eye exam is the best and most effective way to detect glaucoma. The treatment for glaucoma includes prescription eye drops and medicines to lower the pressure in your eye. In some cases, laser treatment or surgery may be effective in reducing pressure.
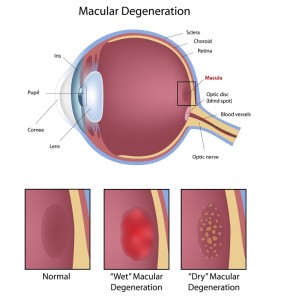
- Age-related macular degeneration (AMD) is a deterioration or breakdown of the macula. The macula is a small area in the retina at the back of the eye that allows you to see fine details clearly in your straight-ahead vision to perform activities such as reading and driving. When the macula does not function correctly, blurriness, dark areas, or distortion can affect your central vision. Macular degeneration affects your ability to see near and far, and can make some activities – like driving, threading a needle, or reading — difficult or impossible.
- Many older people develop macular degeneration as part of the body’s natural aging process. There are 2 types of macular problems, Dry and Wet. Approximately 90% of patients have the Dry form which progresses slowly. Studies have shown that, for people who have dry AMD, vitamins may slow the progression in 20-25% of patients. The Wet form occurs in approximately 10% of patients and can cause bleeding and sudden loss of vision. Macular degeneration is the leading cause of severe vision loss in Caucasians over 65.
- AMD can cause different symptoms in different people. The condition may be hardly noticeable in its early stages. Sometimes only one eye loses vision while the other eye continues to see well for many years. When both eyes are affected, the loss of central vision may be noticed more quickly. Some common ways vision loss is detected: words on a page look blurred; a dark or empty area appears in the center of vision; straight lines (like on a door frame or a picket fence) look distorted.
- The Wet form of macular degeneration can be treated with an injected medication, which is a brief outpatient procedure. At Mt Baker Vision Clinic, we will monitor your with an imaging machine to see if and when a referral for this procedure is needed. This procedure may preserve more sight overall, though it is not a cure, and may not restore vision to normal.
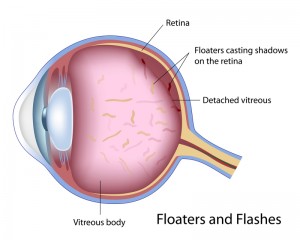
- Flashes and floaters are visual phenomena associated with changes occurring to the back compartment of the eye. Floaters are small dark shapes that appear in your field of vision. Often times they look like squiggly lines, specks or cobwebs that move with eye movement. They are most apparent against light background colors or in well lit areas. Flashing lights can be described as thunderbolts, a spark or an arc of light occurring in the periphery of vision.
- Floaters occur when the vitreous, the jelly in the back of the eye, degenerates or shrinks. As the vitreous shrinks, strands form that cast a shadow upon the retina. While these strands look like they are in front of your eye, they are actually inside your eye. The vitreous tends to degenerate with age. This process is also accelerated in people who are very nearsighted or have incurred ocular trauma among many other causes. A complete breakdown of the vitreous and separation from its attachment to the retina compromise a posterior vitreous detachment. This appears as a large ring-like floater. A small percentage of posterior vitreous detachments are associated with an underlying retinal detachment. Flashes occur when the vitreous is bouncing against or tugging on the retina. This mechanical action produces the perception of a flash of light. Vitreous degeneration and retinal detachment can both trigger symptoms of flashing lights. Since a retinal detachment is a serious vision threatening consequence that can be associated with symptoms of flashing lights and floaters, an examination by your eye doctor is recommended within 24 hours of the onset of symptoms.